Sepsis Awareness – The Facts

The DFW Hospital Council (DFWHC) Foundation has been coordinating the Sepsis Strike Force over the past five years. Led by Patti Taylor, the DFWHC Foundation’s director of quality and patient safety services, the group is made up of representatives from hospitals across North Texas inspired by the goal to create awareness on the dangers of sepsis in our community. Over the next six months leading to Sepsis Awareness Month in September, the Sepsis Strike Force will post blogs and informational graphics across social media to support their 2021 goal of raising community awareness. The Sepsis Strike Force’s journey to September begins today!
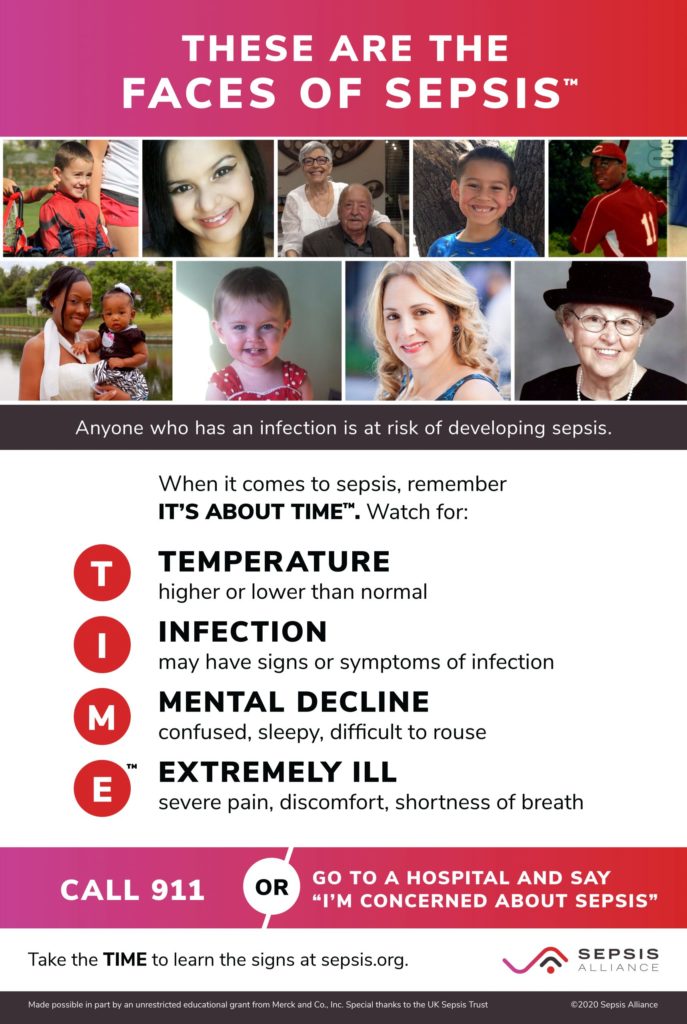
In the U.S., differences in health and mortality are influenced by socio-economic status (SES) and race/ethnicity. Sepsis, the body’s overwhelming and life-threatening response to infection, is no exception.
Sepsis is the leading cause of death in U.S. hospitals and the No. 1 cost of hospitalization at $53 billion annually. More than 1.7 million people in the U.S. are diagnosed with sepsis each year, with an estimated 270,000 deaths annually; more than from prostate cancer, breast cancer and opioid overdoses combined.
Those who survive sepsis have a shortened life expectancy, are more likely to suffer from an impaired quality of life, and often experience worsened mental and physical function.
For the Sepsis Alliance, health equity means eliminating preventable disparities in sepsis incidence, morbidity and mortality. Here’s a few facts on what is known about these disparities, as well as disparities in sepsis awareness and treatment.
Racial/Ethnic disparities in the incidence and mortality of sepsis
• Black and “other nonwhite” individuals have nearly twice the incidence of sepsis as whites.
• Black and Hispanic individuals also have a higher incidence of severe sepsis as compared to whites.
• Blacks bear nearly twice the burden of sepsis deaths relative to the size of the Black population, as compared to whites.
Poverty and Socioeconomic Status
Adults with lower levels of education, income and/or material resources are at greater risk of sepsis mortality. For example:
• Adults below the poverty line have over three to four times the risk of dying of sepsis as compared to adults whose family income is at least five times the poverty line.
• Adult patients without health insurance are more likely to die of sepsis than privately insured patients, and are less than half as likely to be discharged to a nonhospital healthcare facility or discharged with home healthcare.
• Infants from lower income families are 20% more likely to die from sepsis.
• Infants from families without health insurance are three times more likely to die from sepsis.
• Children with severe sepsis or septic shock with public insurance are more likely to die than children with private or other types of insurance.
Awareness and Knowledge
• Sepsis awareness is significantly lower for Blacks than for whites. In a recent survey conducted by Sepsis Alliance, only 49% of respondents identifying as Black had heard the term sepsis, as compared to 76% of white-identifying respondents.
• Income differences were also significantly related to sepsis awareness, with 15% more of the higher income respondents having heard the term ‘sepsis’ as compared to the lower income respondents.
For information, please contact Patti at ptaylor@dfwhcfoundation.org.