Sepsis Awareness 4: Maternal Facts
The DFW Hospital Council (DFWHC) Foundation has been coordinating the Sepsis Strike Force over the past five years. Led by Patti Taylor, the DFWHC Foundation’s director of quality and patient safety services, the group is made up of representatives from hospitals across North Texas inspired by the goal to create awareness on the dangers of sepsis in our community. Over the next six months leading to Sepsis Awareness Month in September, the Sepsis Strike Force will post blogs and informational graphics across social media to support their 2021 goal of raising community awareness.
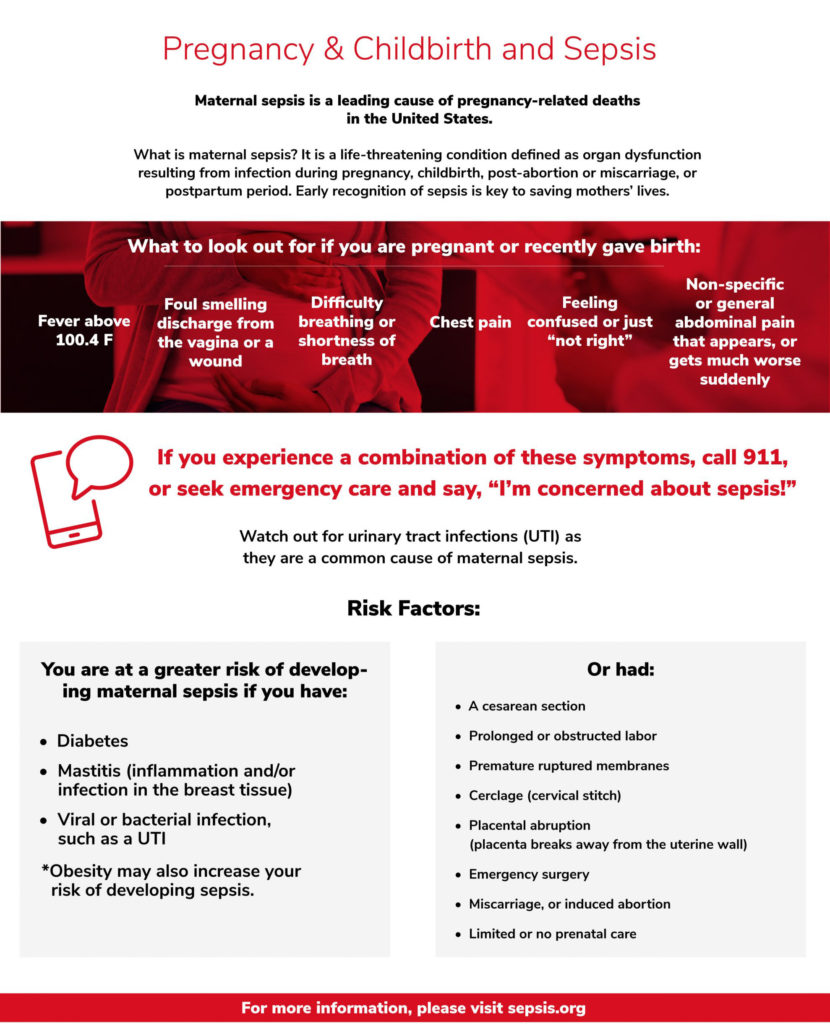
Maternal Sepsis Facts
• The U.S. has the third highest rate of maternal mortality of all high-income countries, with an estimated 2.6 maternal deaths per 10,000 live births.
• Maternal sepsis is estimated to complicate 10 cases per 10,000 live births in the U.S.
• Sepsis causes at least 261,000 maternal deaths every year worldwide, accounting for approximately 11% of all maternal deaths.
• Globally, maternal sepsis is estimated at 5.7 million cases each year.
• In a recent analysis of 52 low, lower-middle, upper-middle and high-income countries, sepsis was estimated to affect 109 women per 10,000 live births. Women from low-income countries were estimated to have the highest rates of sepsis, at 150 women per 10,000 live births.
• Sepsis in pregnancy is associated with an increased risk of preterm birth, prolonged recovery, stillbirth, and maternal death. A recent study found that maternal sepsis was associated with more than 6 times the risk of infant death compared to birth outcomes of healthy mothers.
• The number of cases of maternal sepsis is increasing. One study of the National Inpatient Sample, a national database, reported a 10% annual increase in cases of maternal severe sepsis and sepsis-related deaths in the U.S. between 1998 and 2008.
• Sepsis is driving increases in pregnancy-related deaths in the U.S.5 (Pregnancy-related death is defined as the death of a woman while pregnant or within 1 year of the end of a pregnancy.) According to the CDC, 12.7% of pregnancy-related deaths between 2014 and 2017 were due to infection or sepsis. That makes infection/sepsis the second leading cause of pregnancy-related death.
• Infection is a leading cause of pregnancy-related death at several points in the pregnancy timeline. Infection is the third leading cause of death during pregnancy and in the period 1-6 days after delivery (postpartum). Infection is the leading cause of pregnancy-related death during the period of 7-42 days after delivery. Infection, if not properly treated, can lead to sepsis.
• In the United Kingdom, sepsis accounts for as many as 25% of all maternal deaths.
• More than 50% of women who die from sepsis have one or more chronic co-occurring conditions, including chronic renal (kidney) disease, chronic liver disease and congestive heart failure.
• The Society for Maternal Fetal Medicine recently released new recommendations for the diagnosis and treatment of sepsis, including that sepsis and septic shock be considered medical emergencies. Treatment of sepsis in pregnancy should follow the same basic principles as treatment of patients who are not pregnant.
• The Maternal Mortality Review Committee of the CDC recommends that health facilities have sepsis protocols in place and used by staff members as one strategy to prevent future pregnancy-related deaths.